
The more complete and competent the diagnosis of prostatitis, the more effective the subsequent therapy will be. The approach of a formal physician can result in long-term and ineffective treatment for the patient. Its task is to identify inflammation of the prostate and all the factors that provoke it.
How do doctors diagnose prostatitis
Prostatitis is diagnosed by a urologist or andrologist. After talking with the patient, the doctor prescribes the necessary examinations: first, a standard set (blood, urine, prostate secretions, colon examination), then, if indicated, more detailed and high-tech methods are used: CT, MRI, ultrasound.
Taking anamnesis
During the initial consultation, the doctor will ask the following questions:
- Duration of the relationship (if it became shorter, then under what circumstances);
- Presence of discomfort in the groin during prolonged stay in a static position, as well as after drinking alcohol or hypothermia;
- Frequency and speed of urination (is there any difficulty, intermittent plane, do you have to get up often to use the toilet at night);
- Quality of orgasm (ejaculation still bright or fuzzy, painful).
The more details the patient remembers, the more complete the clinical picture made by the doctor.
Differential Diagnosis
The symptoms of prostatitis are similar to those of a number of other diseases:
- Cystitis (cramps when urinating, pain in the lower abdomen).
- Adenoma (difficulty urinating, feeling of heaviness in the groin).
- Prostate cancer (blood in the urine, problems with urination).
- Pathologies of the rectum: hemorrhoids, paraproctitis (inflammation), anal fissures, crypt (ulcerative colitis).
Additional diagnostic methods and justifications for their use are shown in Table 1.
Table 1. Differential diagnosis of prostatitis
| Disease | Risk group | Analyzes |
|---|---|---|
| Hyperplasia | Men over 45 with no history of urethritis, catheterization, bladder and urethral trauma (circumstances that may explain pain, blood in urine) | Prostate ultrasound and digital examination |
| Prostatiti | Mostly young men who have recently suffered from fever, hypothermia, in whose history there is no provocative factor (identical to hyperplasia) | ultrasound, complete blood count (CBC), digital prostate examination |
| Prostate cancer | Men over 45, no history of provocative factors | Prostate ultrasound, PSA analysis, digital examination |
If necessary, other specialists are involved in the diagnosis: proctologist, neurologist, vertebrologist. The last two specialists identify the causes of pain associated with a violation of the structure of the spine, the violation of nerve endings.
Palpation of the rectum
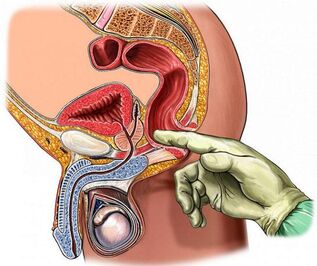
Digital colon examination is the most accessible and informative method for checking the condition of the prostate. During the procedure, the doctor pays attention to the following parameters of his structure:
- Volume;
- Density;
- Surface roughness;
- Homogeneity (tissue homogeneity);
- Boundaries (outline clarity);
- Preservation of the isthmus (longitudinal suture between lobes).
In the prostate, the gland is enlarged due to edema (asymmetry is possible), its stability is elastic, the longitudinal groove (suture) is not palpable and when touched, the patient may feel soreness.
For a clear picture of this type of diagnosisit is necessaryprepare:
- Do not ejaculate the day before, do not drink alcohol, avoid strenuous physical exertion, hypothermia and overheating.
- Do not ride a bicycle for a day, do not use rowing machines (do not injure or massage the prostate this way).
- Before visiting a doctor, have an enema (a micro-enema can be used) to clean the rectal ampoule.
You can feel the prostate at a depth of 3-5 cm from the anus. The doctor performs the procedure with sterile gloves, lubricating the finger with gel. The patient lies on his side with his knees inserted or standing in an elbow-to-knee position.
Laboratory Methods
Laboratory methods for diagnosing prostate inflammation include the study of biomaterials for the presence of pathogens.
Blood
Based on the results of general and biochemical blood tests (take capillaries from the finger), prostatitis can be suspected at an early stage. The analysis is taken on an empty stomach in the morning. You should refrain from smoking one hour before the procedure.
Important indicators:
- Leukocytes (blood cells, the number of which increases with a decrease in immunity against the background of inflammatory reactions). Normally from 4-9 × 10 ^ 9 units;
- ESR (erythrocyte sedimentation rate). The rate is about 5 units, an increase indicates inflammation or an oncological process;
- Lymphocytes. Normally, their percentage of total blood cell volume varies from 18 to 40 units. Excess means infection.
Men over the age of 40 have been assigned a PSA test- a tumor marker whose value exceeds that of chronic prostate or prostate cancer.Norm- less than 4 ng / ml, after 50 years - 5. 53 ng / ml.
Urina
the urethra passes through the prostate (the prostatic part of the urethra), so when the gland becomes inflamed, the urine changes its color and consistency. For the diagnosis of prostatitis, three types of tests are taken:
- General - determination of physical and chemical parameters. Signs of prostate inflammation: urine is cloudy, white, alkaline, has proteins, leukocytes, purulent filaments, sometimes foam or blood. With calcified prostate, phosphates are found.
- Cytological - examination for the presence of pathologically altered cells. The presence of erythrocytes and epithelium may indicate a tumor process.
- Bacteriological - identification of traces of activity of pathogenic microorganisms. To do this, make a tank by planting sediment in a nutrient. If there are bacteria and fungi, then after a while they start to multiply actively. Escherichia coli often provokes prostatitis.
Before shedding urine, you should refrain from eating salty and spicy foods, do not consume alcohol and coloring products (beets, coffee). The analysis is taken in the morning on an empty stomach.For prostatitis, the three-cup test method is used:the patient urinates alternately in each cup; the result is the first, middle and last part. This method allows you to identify the localization of inflammation: urethra, prostate, bladder. The four-cup method is more informative. The last part of the urine is collected after massaging the prostate to get its secretion.
Prostate secretion and sperm
Fluid produced by the prostate gland is a valuable diagnostic material. Prepare for his fence in the same way as for a digital rectal examination. In order for the volume of secretion to be sufficient, you should abstain from sexual intercourse for three to five days.
Methods for examining prostate secretions:
- Microscopy;
- Back planting;
- PCR (polymerase chain reaction).
PCR is the most accurate method. For the processing of biomaterials, special enzymes are used that multiply the number of DNA and RNA fragments of pathogens. Search requires a special device - an amplifier. More precisely, real-time PCR. The result is ready in an hour.
Inflammation of the prostate is indicated by the presence in its fluid of amyloid bodies, staphylococci, streptococci, Pseudomonas aeruginosa, epithelial cells (more than three units in the field of view). The number of lipoid granules decreases, and the number of leukocytes increases.
Thespermogram for prostatitis is an additional test. Against the background of inflammation of the prostate, the sperm becomes yellow or brown, its viscosity increases (liquefies for a long time) and pathogenic microflora is present. In chronic prostatitis are found epithelial cells of the gland, amyloid bodies and mucus.
urethral swab

Urethral swab (scratch) is a less informative method for diagnosing prostatitis than secretion analysis.Used in cases where it is impossible to get the latter due to hemorrhoids, worsening of inflammation, the presence of calcifications in the body of the prostate.
The procedure for obtaining the material is quick but inconvenient: the doctor dips a brush into the urethra, which catches a portion of the cells that cover it along with the microorganisms. The biomaterial is then examined by PCR, which allows you to determine the presence of pathogens in any quantity. The cause of prostatitis can be genital infections: chlamydia, Trichomonas, mycoplasma.
Before doing the test for a day, you should refuse sex, in the morning, perform only external hygienic procedures for the penis (do not spill anything in the urethra), do not urinate for two hours.
Instrumental Methods
Instrumental diagnostic methods allow you to confirm and complete laboratory test results.
Ultrasound and TRUS
Ultrasound examination of the prostate makes it possible to visualize the structure, contours, nature of tissue changes. In the case of prostatitis, transrectal ultrasound (TRUS) is considered the most informative: the doctor inserts a carrier into the rectum. Prepare for the procedure in the same way as for gland palpation. Abdominal ultrasound (through the abdomen) is more comfortable for a man, but the prostate is not fully visible due to the bladder.
With inflammation of the prostate gland, its structure is heterogeneous, the contours are blurred, there may be foci of fibrosis (overcrowded connective tissue), sores. The prostate is enlarged, the groove between its lobes is smooth.
MRI, PET and CT
If the ultrasound gives reason to suspect the presence of a tumor process, then to clarify the picture, the doctor prescribes CT (computed tomography) or MRI (magnetic resonance imaging). The latter type of research is more accurate, but also more expensive. The procedures are painless; in terms of information content, they can replace a biopsy (by removing a tissue fragment).
CT and MRI show in detail the structure of the prostate: stones, cysts, tumors, inflammatory foci, structural abnormalities. For a clearer picture, a contrast agent is pre-injected into a vein (not used for men with renal insufficiency). For the procedure, a suitable type of tomograph and rectal probe is used.
PET - Positive Emission CT. Allows you to analyze the state of the prostate at the cellular and molecular level. It determines not only the presence and size of the tumor, but also the speed and quality of metabolic processes occurring in it.
Regarding the preparation:the rectum should be emptied. Do not eat for five hours before the procedure.
Diagnostic features of certain types of prostatitis
Acute bacterial (infectious) prostatitis is diagnosed based on patient complaints, urine analysis, ultrasound, urethral staining. With active inflammation, the gland is painful, transrectal interventions are not allowed, in extreme cases, a careful examination of the finger.
Laboratory data for the diagnosis of acute prostatitis are not particularly informative. A urine culture may be advisable but not required. With active inflammation, there is no time to wait for results. To alleviate the symptoms, broad-spectrum antibacterial therapy is performed.
Chronic prostatitis is practically not manifested in any way, therefore, its detection requires a whole range of laboratory, physical, instrumental methods. Determination of the patient's immune and neurological status may be required.
Palpation of the gland, urine and prostatic secretions are of key importance. The presence of more than 10 leukocytes in the visual field indicates inflammation. If the bacterial culture does not give the growth of infectious microflora against the background of an increased number of leukocytes, then an analysis for genital infections is necessary.
With the bacterial nature of inflammation in the urine and prostate fluid, a large number of pathogens are found. An undeniable microbiological sign of chronic inflammation: the number of microbes (CFU) is more than 104 per ml. Some of them are numbered in the tens, so their presence in an amount from 10 to 102 per ml may indicate prostate.
In abacterial (non-infectious) inflammation, they are absent, but experts recommend in such cases to do a more in-depth analysis: prostate puncture, through which pathogens living in closed prostate pathways are extracted. At the same time, the bacterial culture is sterile, but the pathogen is still found at the bottom. Most often it is one of the varieties of E. coli.
Ultrasound does not always show chronic inflammation. In addition to the above methods, the doctor may prescribe uroflowmetry - measurement of urine flow using special sensors.
Typical interruptions
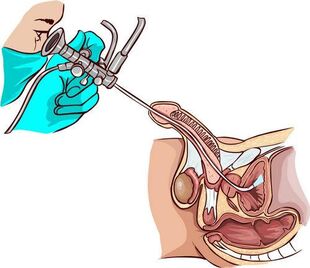
For chronic long-term prostate with signs of coliculitis (inflammation of the seminal tubercle near the prostate),uses urethroscopy - a visual examination of the canal using an endoscopic device. Helps to identify narrowing of the urethra, violations of its structure, the state of the mouth of the prostate excretory ducts (mucus, pus, thickening) and seminal tubercle.
Interpretation of results (determination of prostate stages from seminal tuberculosis condition):
- First: seminal tuberculosis is red, edematous, bleeding. The same pattern is observed in the back of the urethra;
- Second: periodic increase and decrease of redness and swelling is characteristic;
- Third: scarring occurs in the tissues of the tubercle and urethra, due to which the lumen of the urethra may narrow (narrowing).
Ureteroscopy irritates the receptors of the seminal tubercle, which leads to impaired microcirculation and motility of the prostate, so the procedure is not performed unnecessarily.
Cystitis is also an accompaniment to chronic prostatitis. Inflammation of the bladder walls is detected by ultrasound andcystoscopy. During the research, pathological changes in the mucous membranes are determined, especially in the neck area. Bladder condition in the background of chronic prostatitis (prostate sclerosis):
- Cicatricial deformation of the bladder triangle.
- Enlarged urethra.
- Narrowing of the neck.
Cystoscopy is already described in the final stage of examination in the presence of lower abdominal pain and frequent urination.
The most difficult to diagnose is chronic abacterial prostatitis with pelvic pain of undetermined origin. In such patients, physicians primarily conduct research to rule out cystitis and neuropsychiatric pathologies.
How to diagnose prostatitis at home
A man may suspect an acute prostate from the following signs:
- Severe pain in the lower abdomen and groin (between the testicles and anus);
- Increased body temperature;
- Pain when urinating (like cystitis);
- Early and painful ejaculation.
The same symptoms appear during exacerbations of chronic prostatitis, provoked by hypothermia or alcohol intake. The development of this form of pathology can be evidenced by the periodic appearance of blood in the urine, dull pain in the perineum (especially in a static position), difficulty urinating, worsening of erection. Such signs are the reason to contact a urologist.
Conclusion
The longer the inflammatory process in the prostate lasts, the more difficult the treatment will be, so you should not delay the diagnosis. In government agencies, most procedures and follow-up treatment are free.
























